Superior mesenteric artery syndrome refers to obstruction at the level of the third portion of the duodenum as it passes between the superior mesenteric artery and the aorta. The obstruction may be due to narrowing of the aorta-superior mesenteric artery distance or inadequate peristaltic pressure to pass food past this area (as could be seen with scleroderma, for example).
Superior mesenteric artery syndrome is classically described in patients with rapid weight loss, those on bed rest, or patients with prior abdominal surgery, but can be seen with scleroderma, diabetes, pancreatitis, peptic ulcers, and malignant lymph nodes or tumors in the root of the mesentery. Aortic or superior mesenteric artery aneurysms or atherosclerotic disease can also cause narrowing of the aorta-superior mesenteric artery distance.
Upper gastrointestinal series may show gastric and duodenal dilatation with retention of barium, and extrinsic pressure on the third part of the duodenum (arrow).
A classically described finding is a linear cut-off of contrast at the proximal third portion of the duodenum,
which is to the right of the spine. However, the superior mesenteric artery is central or slightly to the
left of midline (as clearly demonstrated on CT), so the anatomic origin of this finding is not clear to me.
CTA is the modality of choice for this rare diagnosis. The aorta-superior mesenteric artery angle and the distance between the aorta and superior mesenteric artery, and the third portion of the duodenum can be assessed on CTA.
In normal patients, the aorta-superior mesenteric artery angle is between 25°-60°, and the aorta-superior mesenteric artery distance is between 10 mm - 28 mm.
Patients with superior mesenteric artery syndrome have angles between about 5° to 20° and aorta-superior meseteric artery distances between 2 mm and 8 mm.
In our patient, the aorta-superior mesenteric artery angle was about 15° and the aorta-superior mesenteric artery distance was about 5 mm.
References
- Gondos B. Duodenal compression defect and the "superior mesenteric artery syndrome". Radiology. 1977 Jun;123(3):575-80.
- Mindell HJ, Holm JL. Acute superior mesenteric artery syndrome. Radiology. 1970 Feb;94(2):299-30
- Horton KM, Fishman EK. CT angiography of the mesenteric circulation. Radiol Clin North Am. 2010 Mar;48(2):331-45, viii.
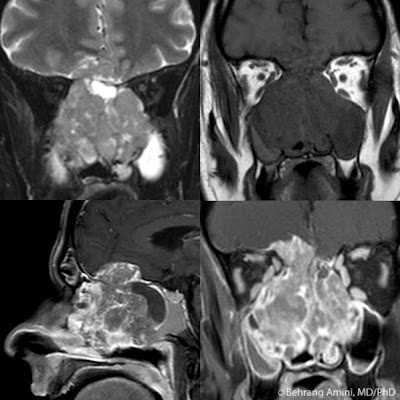
 Astrocytomas are the most common primary, solitary, supratentorial brain lesion in adults (all these qualifiers are meant to hide the fact that brain lesions are most commonly metastases). The World Health Organization classifies them into 4 grades.
Astrocytomas are the most common primary, solitary, supratentorial brain lesion in adults (all these qualifiers are meant to hide the fact that brain lesions are most commonly metastases). The World Health Organization classifies them into 4 grades.